Canine Cataracts
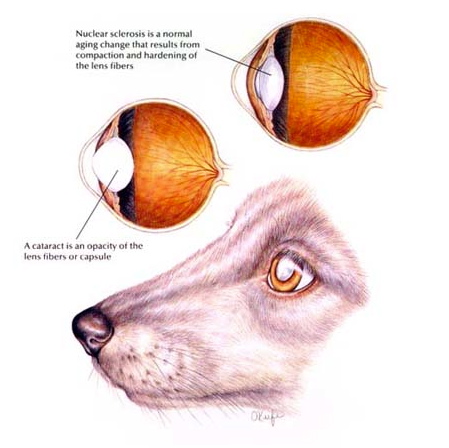
A cataract is any opacity in the normally clear crystalline lens of the eye. A cataract can be small or focal and not interfere with vision, or it can progress and involve more of the lens resulting in troubled vision or blindness in the affected pet. Advanced or complete cataracts may also cause the pupil to appear cloudy. Cataracts are differentiated from nuclear or lenticular sclerosis in that they are a true opacity through which light cannot pass.
Causes
There are many causes of cataracts in dogs, but most commonly the condition is inherited. While almost every purebred is susceptible to inherited cataracts, certain breeds are over-represented including the Bichon Frise, Cocker Spaniel, Poodle, Yorkie, and most Poodle crosses. Other causes of cataracts include diabetes mellitus, chronic inflammatory conditions (anterior uveitis), trauma, and aging.
In contrast to dogs, diabetes mellitus is not a common cause of cataracts in cats. Chronic inflammation (uveitis) is the most common cause of cataracts in cats and horses.
Diagnosis
The diagnosis is generally based on the findings of an eye examination. Depending on the extent of progression, the normally black pupil may take on a white or cloudy appearance, and the animal’s vision may become affected, causing it to bump into things. Complete or advanced cataracts are one cause of poor vision or blindness. In instances where the internal structures of the eye cannot be visualized or inspected, other tools such as ultrasound (sonogram) of the eye may be necessary to determine if a cataract is present.
When a cataract is diagnosed (even in the early stages), a consultation with a veterinary ophthalmologist should be considered. A specialist can evaluate the overall health of the eye and determine the presence of inflammation, glaucoma, and any disorders of the associated structures of the eye, including concurrent retinal degeneration. This provides the pet owner the opportunity to learn more about their pet's situation, prognosis for long-term vision, and discuss whether cataract surgery might be an option for that pet in the near or distant future.
Newly diagnosed animals with diabetes mellitus
- Owners should be aware that 75 to 85 percent of dogs will develop complete cataracts within the first year of being diagnosed
- Owners should monitor their pet's eyes for cloudiness, redness, and any indication of irritation including squinting or rubbing, and report changes to their veterinarian immediately
- Periodic recheck exams should be scheduled as recommended by the veterinarian
- Veterinarians should suggest an ophthalmology consult as soon as cataracts are identified
- If the intraocular pressures (IOP) are normal at the time of diagnosis, it is often recommended to prescribe treatment with a topical anti-inflammatory and recheck the eyes on a regular basis. Secondary glaucoma does frequently arise in association with cataracts, therefore, frequent monitoring of patient IOP is recommended. Elevation in IOP (glaucoma) requires additional medical or possibly surgical therapy.
It is important to understand that progressive cataracts can eventually cause additional damage to the eye. Addressing the cataract is an important step to limiting long-term complications that may compromise the comfort and potential for vision of an affected eye.
Treatment
- Medical
Regardless of the cause, the first step in managing a patient with a cataract is to reduce and / or prevent cataract-induced intraocular inflammation, also called lens-induced uveitis. With the formation of cataracts, lens proteins can be released into the anterior chamber. Due to the antigenic nature of these proteins, inflammation can ensue. This uveitis (if not properly managed) can lead to complications including secondary glaucoma, retinal detachment, corneal edema, posterior synechia (adhesions) and, ultimately, can prevent the dog from being considered a candidate for cataract surgery.
- Surgery
The only definitive treatment for cataracts is surgical removal. In considering the pet for cataract surgery, assessment of retinal health is recommended for most patients to ensure they are good candidates for surgery. This is accomplished by conducting two tests:
- electroretinogram (ERG) which measures the electrical activity in the retina and evaluates the pet for concurrent retinal degeneration
- ocular ultrasound to screen for retinal detachment and vitreous abnormalities
There are a couple of different surgical techniques for achieving removal of the opaque lens.
Phacoemulsification
This advanced technology uses high-speed ultrasound waves coupled with aspiration to break up the cataract and remove the lens material from the eye. This technique generally allows for shorter surgery times, minimizes intraocular trauma and has higher post-operative success rates compared with other techniques. In good surgical candidates, this technique approaches a 95 percent or greater success rate.
Extracapsular Lens Extraction
This procedure involves making a larger incision and applying a different technique for manually extracting the cataractous lens. This technique is often employed when complications develop during phacoemulsification. The success rate can be impacted by several different factors, but is generally around 80 to 85 percent.
Intracapsular Lens Extraction
This technique is used when instablility of the lens is encountered or when dislocation of the lens occurs due to breakage of lens zonules. The greatest complication seen with this technique is the development of glaucoma or retinal detachment.
- Lens Implant
After the cataract is removed, the vision in the pet is blurry (far-sighted) because the focusing power of they eye is lost without the lens. To restore clear vision, an artificial lens can be implanted at the time of surgery. This implant (intraocular lens) is inserted into the lens capsule (sac) that remains after the cataract is removed. In instances where the sac is unhealthy or has been removed altogether (intracapsular technique), the lens implant can be sutured in place within the eye. In some instances, the surgeon may elect not to implant an artificial lens. Without a lens implant, and if the surgery is successful, the pet's vision is restored, however the impact of blurriness on the pet's function is variable.
Post-op care
Success of cataract surgery is highly dependent on the postoperative care provided to the pet. A typical treatment plan after surgery includes administration of oral and topical eye medications to prevent infection and control intraocular pressure, inflammation and pain. Use of an Elizabethan collar is recommended to prevent rubbing of the operated eye(s) and periodic recheck examinations are required to monitor healing.
Prognosis
Cataracts are progressive and can lead to anterior uveitis, lens capsule rupture, glaucoma, retinal detachment, and blindness. Early detection and intervention for patients with cataracts will significantly reduce complications and improve the final outcome.
Early surgical intervention has excellent success rates - 95 percent or greater. The risks and potential complications increase with the chronicity and severity of the cataract. Surgical intervention with long-standing hypermature cataracts can be unrewarding due to the increased risk of retinal detachment and glaucoma.
Illustration reprinted with permission by the copyright owner, Hill’s Pet Nutrition, Inc.
